
- Home
- About
- Services
- Specialists
- Research
- Achivements
- gallery
- contact








- Home
- About Us
- Orthopedics
- Know Your Alignment
- Sports Medicine
- Knee
- Arthroscopic ACI Cartilage Transplant
- Arthroscopic ACL Avulsion Fixation
- Arthroscopic ACL Primary Repair
- Arthroscopic ACL Reconstruction – All Inside Technique
- Arthroscopic ACL Rehab
- Arthroscopic ACL Revision Surgery
- Arthroscopic ACL Single Bundle Reconstruction
- Arthroscopic assisted MPFL Reconstruction
- Arthroscopic assisted Multiple Ligament Tear – SURGERY
- Arthroscopic Medial Meniscal Repair
- Arthroscopic OATS Chondroplasty
- Arthroscopic OCD Fixation
- Arthroscopic Paediatric ACL Reconstruction
- Arthroscopic PCL Avulsion Fixation
- Arthroscopic PCL Reconstruction
- Arthroscopy Assisted STEM Cell Cartilage Transplant
- PCL Rehabilitation
- Total Knee Replacement
- Shoulder
- Arthroscopic Rotator Cuff Repair
- Arthroscopic Bankart Repair
- Arthroscopy Assisted Latarjet Surgery
- AC Joint Fixation
- Arthroscopic Capsular Release
- Arthroscopic Sub – Acromial Decompression (SAD)
- Arthroscopic Calcific Tendinitis Excision
- Arthroscopic Biceps Tenodesis
- Arthroscopic SLAP Repair
- Arthroscopic Revision Cuff Repair
- Arthroscopic Revision Bankart Repair
- Shoulder Rehab
- Elbow
- Wrist
- Hip
- Ankle
- Our Specialities
- Cardiology
- Gastroenterology
- Radiology
- Internal Medicine & Diabetology
- Anesthesiology & Intensive Care Unit
- Neurology
- Nephrology
- Urology
- Oncology
- Rheumatology
- Endocrinology
- General Surgery
- Laparoscopic Surgery
- Podiatric / Diabetic Foot Clinic
- Obstetrics & Gynecology
- ENT
- Plastic & Cosmetic Surgery
- Paediatrics
- Pulmonology
- Psychiatry
- Vascular Surgery
- Dermatology
- Oral and Maxillofacial Surgery
- Our Services
- Resource
- Enquiry


- Home
- About Us
- Orthopedics
- Know Your Alignment
- Sports Medicine
- Knee
- Arthroscopic ACI Cartilage Transplant
- Arthroscopic ACL Avulsion Fixation
- Arthroscopic ACL Primary Repair
- Arthroscopic ACL Reconstruction – All Inside Technique
- Arthroscopic ACL Rehab
- Arthroscopic ACL Revision Surgery
- Arthroscopic ACL Single Bundle Reconstruction
- Arthroscopic assisted MPFL Reconstruction
- Arthroscopic assisted Multiple Ligament Tear – SURGERY
- Arthroscopic Medial Meniscal Repair
- Arthroscopic OATS Chondroplasty
- Arthroscopic OCD Fixation
- Arthroscopic Paediatric ACL Reconstruction
- Arthroscopic PCL Avulsion Fixation
- Arthroscopic PCL Reconstruction
- Arthroscopy Assisted STEM Cell Cartilage Transplant
- PCL Rehabilitation
- Total Knee Replacement
- Shoulder
- Arthroscopic Rotator Cuff Repair
- Arthroscopic Bankart Repair
- Arthroscopy Assisted Latarjet Surgery
- AC Joint Fixation
- Arthroscopic Capsular Release
- Arthroscopic Sub – Acromial Decompression (SAD)
- Arthroscopic Calcific Tendinitis Excision
- Arthroscopic Biceps Tenodesis
- Arthroscopic SLAP Repair
- Arthroscopic Revision Cuff Repair
- Arthroscopic Revision Bankart Repair
- Shoulder Rehab
- Elbow
- Wrist
- Hip
- Ankle
- Our Specialities
- Cardiology
- Gastroenterology
- Radiology
- Internal Medicine & Diabetology
- Anesthesiology & Intensive Care Unit
- Neurology
- Nephrology
- Urology
- Oncology
- Rheumatology
- Endocrinology
- General Surgery
- Laparoscopic Surgery
- Podiatric / Diabetic Foot Clinic
- Obstetrics & Gynecology
- ENT
- Plastic & Cosmetic Surgery
- Paediatrics
- Pulmonology
- Psychiatry
- Vascular Surgery
- Dermatology
- Oral and Maxillofacial Surgery
- Our Services
- Resource
- Enquiry



- Home
- About Us
- Orthopedics
- Know Your Alignment
- Sports Medicine
- Knee
- Arthroscopic ACI Cartilage Transplant
- Arthroscopic ACL Avulsion Fixation
- Arthroscopic ACL Primary Repair
- Arthroscopic ACL Reconstruction – All Inside Technique
- Arthroscopic ACL Rehab
- Arthroscopic ACL Revision Surgery
- Arthroscopic ACL Single Bundle Reconstruction
- Arthroscopic assisted MPFL Reconstruction
- Arthroscopic assisted Multiple Ligament Tear – SURGERY
- Arthroscopic Medial Meniscal Repair
- Arthroscopic OATS Chondroplasty
- Arthroscopic OCD Fixation
- Arthroscopic Paediatric ACL Reconstruction
- Arthroscopic PCL Avulsion Fixation
- Arthroscopic PCL Reconstruction
- Arthroscopy Assisted STEM Cell Cartilage Transplant
- PCL Rehabilitation
- Total Knee Replacement
- Shoulder
- Arthroscopic Rotator Cuff Repair
- Arthroscopic Bankart Repair
- Arthroscopy Assisted Latarjet Surgery
- AC Joint Fixation
- Arthroscopic Capsular Release
- Arthroscopic Sub – Acromial Decompression (SAD)
- Arthroscopic Calcific Tendinitis Excision
- Arthroscopic Biceps Tenodesis
- Arthroscopic SLAP Repair
- Arthroscopic Revision Cuff Repair
- Arthroscopic Revision Bankart Repair
- Shoulder Rehab
- Elbow
- Wrist
- Hip
- Ankle
- Our Specialities
- Cardiology
- Gastroenterology
- Radiology
- Internal Medicine & Diabetology
- Anesthesiology & Intensive Care Unit
- Neurology
- Nephrology
- Urology
- Oncology
- Rheumatology
- Endocrinology
- General Surgery
- Laparoscopic Surgery
- Podiatric / Diabetic Foot Clinic
- Obstetrics & Gynecology
- ENT
- Plastic & Cosmetic Surgery
- Paediatrics
- Pulmonology
- Psychiatry
- Vascular Surgery
- Dermatology
- Oral and Maxillofacial Surgery
- Our Services
- Resource
- Enquiry
Importance of Regular Kidney Checkups – Early Signs of Kidney Damage

Your kidneys work around the clock to filter waste and keep your body healthy, but kidney disease often develops silently without obvious symptoms until it’s too late. Regular kidney checkups can catch problems early when they’re still treatable, potentially saving your life and preventing the need for dialysis or transplant.
This guide is for anyone concerned about their kidney health, especially those with diabetes, high blood pressure, family history of kidney disease, or other risk factors. We’ll explore the early warning signs that demand immediate attention and explain the life-saving benefits of regular kidney screenings that can detect problems before they become serious.
Understanding Your Kidneys and Their Vital Functions
How Kidneys Filter Waste and Toxins From Your Blood
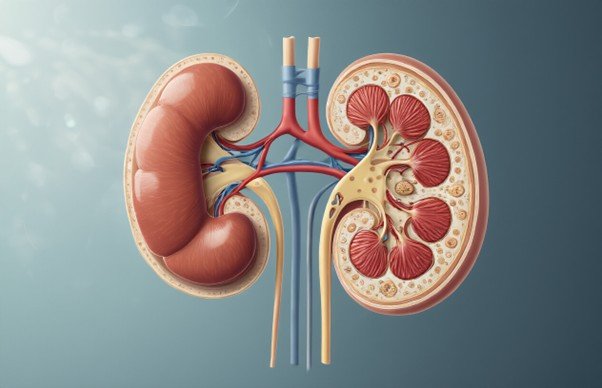
Your kidneys work like incredibly sophisticated filtration systems, processing about 50 gallons of blood every single day. Think of them as your body’s personal water treatment plant, running 24/7 without a break. Each kidney contains roughly one million tiny filtering units called nephrons, and each nephron has its own microscopic filter called a glomerulus.
When blood flows through these glomeruli, they act like super-fine sieves, allowing water and small molecules to pass through while keeping larger, important substances like proteins and blood cells in your bloodstream. The filtered liquid then travels through a series of tubes where your kidneys decide what to keep and what to toss out.
Your kidneys are surprisingly smart about this process. They reabsorb about 99% of the water they initially filter, along with essential nutrients like glucose and amino acids. Meanwhile, they collect waste products like urea, creatinine, and excess salts for elimination through urine. This constant cleaning process prevents toxic buildup that would otherwise poison your entire system within days.
Role in Maintaining Fluid Balance and Blood Pressure
Your kidneys serve as master regulators of your body’s fluid levels, constantly adjusting how much water you retain or eliminate. When you’re dehydrated, they conserve water by producing concentrated urine. When you’ve had too much to drink, they increase urine production to prevent dangerous fluid overload.
This fluid regulation directly impacts your blood pressure through several mechanisms. Your kidneys control blood volume by adjusting how much sodium and water they retain. More fluid in your bloodstream means higher blood pressure, while less fluid results in lower pressure. They also produce renin, an enzyme that triggers a cascade of reactions leading to blood vessel constriction when blood pressure drops.
Hormone Production for Red Blood Cell Creation
Your kidneys moonlight as hormone factories, producing erythropoietin (EPO), a crucial hormone that tells your bone marrow when to ramp up red blood cell production. When kidney cells detect low oxygen levels in your blood, they release EPO like an emergency signal, prompting your bone marrow to create more oxygen-carrying red blood cells.
This process explains why people with kidney disease often develop anemia. As kidney function declines, EPO production drops, leading to fewer red blood cells and reduced oxygen delivery throughout the body. Patients may experience fatigue, weakness, and shortness of breath as their blood’s oxygen-carrying capacity diminishes.
Your kidneys also help activate vitamin D, transforming it into calcitriol, the active form your body can actually use. This hormone regulates calcium absorption in your intestines and maintains proper calcium and phosphorus levels in your blood, keeping your bones strong and healthy.
Regulation of Electrolytes and Acid-Base Balance
Your kidneys maintain a delicate chemical balance that keeps your body functioning properly. They carefully regulate electrolyte levels, including sodium, potassium, chloride, and phosphorus, making minute adjustments based on what you eat and how your body functions.
Potassium regulation deserves special attention because too much or too little can cause dangerous heart rhythm problems. Your kidneys fine-tune potassium levels by increasing or decreasing how much they excrete in urine. They also manage calcium and phosphorus balance, working closely with parathyroid hormone and vitamin D.
Perhaps most critically, your kidneys maintain your blood’s pH level within an extremely narrow range of 7.35 to 7.45. They accomplish this by controlling how much acid your body eliminates and by producing bicarbonate, a natural buffer that neutralizes excess acid. When this balance tips in either direction, cellular function suffers dramatically, potentially leading to coma or death.
Hidden Dangers of Undetected Kidney Disease
Silent Progression Without Obvious Symptoms
Chronic kidney disease earns its reputation as a “silent killer” because it can advance for years without producing any noticeable symptoms. Your kidneys are remarkably resilient organs that continue functioning even when significantly damaged. They can lose up to 90% of their capacity before you experience any obvious warning signs.
During the early stages, your kidneys compensate for damaged tissue by working harder. The remaining healthy nephrons (filtering units) increase their workload to maintain normal waste removal and fluid balance. This compensation mechanism masks the underlying damage, creating a false sense of security.
People often feel completely normal while their kidney function steadily declines. Blood pressure may remain stable, energy levels seem fine, and daily activities continue without interruption. This deceptive period can last months or even years, allowing irreversible damage to accumulate silently.
The absence of pain compounds this problem. Unlike other organs that signal distress through discomfort, kidneys rarely hurt when diseased. You won’t experience the sharp warning that accompanies a heart attack or the obvious symptoms of a broken bone. This painless deterioration means many people only discover their kidney disease when it has progressed to advanced stages.
Irreversible Damage Before Noticeable Signs Appear
Once kidney damage occurs, it cannot be reversed or repaired. Scar tissue replaces healthy kidney tissue permanently, reducing the organ’s filtering capacity forever. By the time symptoms become apparent, substantial and irreversible damage has already occurred.
The first noticeable symptoms typically appear when kidney function drops below 30% of normal capacity. At this point, waste products begin accumulating in your blood, causing:
- Persistent fatigue and weakness
- Swelling in legs, ankles, or around the eyes
- Difficulty concentrating
- Decreased appetite
- Changes in urination patterns
When these symptoms finally emerge, you’ve already lost approximately 70% of your kidney function. The damage that occurred during the silent phase cannot be undone, even with aggressive treatment. Medical interventions can only slow further progression and manage complications.
This timing creates a narrow window for prevention. Regular screening catches problems while treatment can still preserve remaining kidney function. Waiting for symptoms means accepting permanent disability and preparing for eventual dialysis or transplantation.
The progressive nature of kidney disease means that once damage begins, it often accelerates. Each nephron that fails places additional stress on surviving nephrons, creating a cycle of increasing damage. Early detection and intervention can break this cycle before it becomes unstoppable.
Increased Risk of Cardiovascular Complications
Kidney disease dramatically increases your risk of heart attack, stroke, and other cardiovascular problems. Even mild kidney dysfunction doubles your risk of dying from heart disease. As kidney function declines, cardiovascular risk continues to climb exponentially.
Your kidneys play a crucial role in regulating blood pressure, managing fluid balance, and controlling electrolyte levels. When they malfunction, these systems become disrupted, placing enormous strain on your cardiovascular system.
Damaged kidneys struggle to remove excess sodium and fluid from your body, leading to high blood pressure. This hypertension forces your heart to work harder and damages blood vessels throughout your body. The combination creates a dangerous feedback loop where kidney damage worsens heart health, and poor heart health accelerates kidney decline.
Kidney disease also disrupts the production of hormones that regulate red blood cell production and bone health. Anemia develops as kidney function declines, reducing oxygen delivery to your heart and other vital organs. Mineral imbalances affect heart rhythm and increase the risk of sudden cardiac death.
People with kidney disease often die from cardiovascular complications before their kidneys fail completely. This makes early detection and cardiovascular protection essential components of kidney disease management. Regular monitoring allows doctors to implement protective strategies before irreversible damage occurs.
Early Warning Signs That Demand Immediate Attention

Changes in urination patterns and frequency
Your kidneys work around the clock to filter waste and excess fluid from your blood, so any changes in your bathroom habits could be their way of sending up a red flag. When kidney function starts to decline, you might notice you’re running to the bathroom more often than usual, especially during the night. Some people experience the opposite problem – producing much less urine than normal, which can be equally concerning.
Pay attention to sudden changes in how often you need to urinate. If you’re waking up multiple times during the night when you used to sleep through, or if you’re constantly feeling the urge to go but only producing small amounts, these could be early warning signs. The color and smell of your urine matter too – dark, concentrated urine or urine with an unusual odor can signal that your kidneys aren’t working properly.
Unexplained swelling in legs, ankles, or face
When your kidneys can’t effectively remove excess fluid from your body, that fluid has to go somewhere. Swelling, medically known as edema, often shows up first in your feet and ankles because gravity pulls the extra fluid downward. You might notice your shoes feeling tighter than usual or sock marks leaving deeper impressions on your skin.
Facial swelling, particularly around the eyes, can be another telltale sign. Many people wake up with puffy eyes and dismiss it as a bad night’s sleep, but persistent facial swelling could indicate your kidneys are struggling. The swelling might also appear in your hands, making rings feel tight or causing your fingers to look puffy.
This type of swelling doesn’t go away with rest or elevation like normal swelling might. If you press on the swollen area and it leaves an indentation that takes time to bounce back, this is called “pitting edema” and warrants immediate medical attention.
Persistent fatigue and weakness
Healthy kidneys produce a hormone called erythropoietin, which tells your bone marrow to make red blood cells. When kidney function declines, your body produces fewer red blood cells, leading to anemia. This condition leaves you feeling constantly tired, even after a full night’s sleep.
The fatigue associated with kidney problems isn’t just ordinary tiredness – it’s a deep, persistent exhaustion that interferes with daily activities. You might find yourself struggling to climb stairs, feeling breathless during light exercise, or needing frequent naps. Some people describe it as feeling like their energy has been completely drained.
This exhaustion often comes with weakness and difficulty concentrating. Tasks that once seemed effortless become challenging. If you’re getting adequate sleep but still feeling wiped out for weeks at a time, your kidneys might be crying out for help.
High blood pressure that’s difficult to control
Your kidneys and blood pressure have a complex relationship – damaged kidneys can cause high blood pressure, and high blood pressure can damage your kidneys. This creates a dangerous cycle where each problem makes the other worse. When kidney disease is developing, you might notice your blood pressure readings creeping up despite taking medication or following lifestyle recommendations.
If you’ve never had blood pressure issues before but suddenly develop hypertension, or if your previously well-controlled blood pressure becomes difficult to manage, kidney problems could be the culprit. Your doctor might need to add more medications or increase dosages, yet your numbers remain stubbornly high.
Regular blood pressure monitoring becomes especially important if you have risk factors for kidney disease. Some people don’t experience obvious symptoms of high blood pressure, which is why it’s often called the “silent killer.”
Foamy or bloody urine appearance
Changes in urine appearance can provide valuable clues about kidney health. Foamy or bubbly urine that looks like beer foam might indicate protein in your urine, a condition called proteinuria. Healthy kidneys keep protein in your blood where it belongs, but damaged kidney filters allow protein to leak into your urine.
Blood in your urine can range from obvious red coloring to a darker, tea-colored appearance. Sometimes the blood isn’t visible to the naked eye but shows up in lab tests. Any blood in your urine deserves immediate medical evaluation, as it could indicate serious kidney damage or other urinary tract problems.
Don’t ignore these visual changes or assume they’ll resolve on their own. While foamy urine might occasionally occur due to dehydration or vigorous urination, persistent changes warrant professional evaluation. Taking a photo with your phone can help you show your healthcare provider exactly what you’re seeing.
Life-Saving Benefits of Regular Kidney Screenings
Early Detection Prevents Advanced Kidney Disease
Regular kidney screenings act as your first line of defense against irreversible kidney damage. When caught in the earliest stages, kidney disease often shows subtle changes that can be detected through simple blood and urine tests before you experience any symptoms. These screenings can identify problems when your kidney function drops to 90% of normal capacity, giving you a significant window for intervention.
The beauty of early detection lies in its ability to catch chronic kidney disease (CKD) during stages 1 and 2, when the damage is minimal and often reversible with proper treatment. At this point, your kidneys still function well enough to maintain your body’s normal processes, but the screening reveals warning signs like protein in your urine or slightly elevated creatinine levels. Without these routine checks, kidney disease typically remains silent until it reaches stage 3 or 4, when 50-85% of kidney function has already been lost.
Timely Intervention Slows Disease Progression
Once kidney problems are identified early, medical interventions can dramatically slow the progression of disease. Your healthcare team can immediately address underlying causes such as high blood pressure, diabetes, or medication toxicity that may be damaging your kidneys. Blood pressure medications like ACE inhibitors or ARBs specifically protect kidney function while controlling hypertension.
Dietary modifications play a crucial role in this intervention phase. Reducing protein intake, limiting sodium, and managing phosphorus levels can significantly reduce the workload on your kidneys. When combined with tight blood sugar control for diabetic patients, these interventions can slow kidney function decline by 30-50% compared to untreated progression.
Regular monitoring also allows doctors to adjust medications that might harm your kidneys and optimize treatments for conditions like anemia and bone disease that commonly accompany kidney problems.
Reduced Need for Dialysis or Transplantation
The most compelling benefit of regular screening is avoiding the need for life-altering treatments like dialysis or kidney transplantation. Studies show that patients who receive consistent kidney monitoring and early treatment can delay or completely avoid end-stage renal disease by 10-15 years compared to those whose kidney disease goes undetected.
When kidney function drops below 15%, dialysis becomes necessary to filter toxins from your blood – a treatment that requires 3-4 sessions per week, each lasting 3-4 hours. Transplantation, while life-saving, involves major surgery, lifelong immunosuppressive medications, and the constant search for compatible donors.
Early intervention through regular screenings allows many people to maintain kidney function at levels that don’t require these intensive treatments, preserving quality of life and independence.
Lower Healthcare Costs Through Preventive Care
Preventive kidney care delivers enormous cost savings compared to treating advanced kidney disease. A basic kidney screening panel costs between $50-100 and includes blood tests for creatinine, blood urea nitrogen, and urinalysis. Annual screenings for high-risk individuals represent a minimal investment with maximum returns.
The financial impact becomes staggering when kidney disease progresses to end-stage renal disease. Dialysis costs average $89,000 annually, while kidney transplantation can exceed $300,000 in the first year alone. Medicare and insurance companies recognize these savings, which is why they typically cover preventive kidney screenings at 100% for qualifying patients.
Beyond direct medical costs, early detection prevents the indirect expenses associated with missed work, disability, and reduced earning capacity that often accompany advanced kidney disease.
Essential Tests Your Doctor Should Perform
Blood tests measuring creatinine and GFR levels
Your doctor will order a comprehensive metabolic panel that includes serum creatinine levels and estimated glomerular filtration rate (eGFR). Creatinine is a waste product your muscles produce naturally, and healthy kidneys filter it out of your blood efficiently. When kidney function declines, creatinine builds up in your bloodstream.
The eGFR calculation takes your creatinine level and factors in your age, sex, and race to estimate how well your kidneys are filtering waste. Normal eGFR levels range from 90-120 mL/min/1.73m², while readings below 60 for three months or more signal chronic kidney disease.
Blood urea nitrogen (BUN) is another crucial marker that measures urea, a waste product from protein breakdown. Elevated BUN levels often accompany rising creatinine when kidney function deteriorates.
Urinalysis detecting protein and blood traces
A simple urine test reveals critical information about kidney health that blood tests might miss. Healthy kidneys prevent protein from leaking into urine, so finding protein (proteinuria) signals kidney damage even when other tests appear normal.
Microalbuminuria testing detects tiny amounts of albumin protein in urine – often the first sign of diabetic kidney disease. This test is especially important for people with diabetes or high blood pressure.
Red blood cells in urine (hematuria) can indicate kidney stones, infections, or more serious conditions like glomerulonephritis. White blood cells suggest infection or inflammation.
Your doctor will also check for:
- Glucose levels (diabetes indicator)
- Specific gravity (kidney concentration ability)
- Casts and crystals (kidney damage markers)
- Bacteria or abnormal cells
Blood pressure monitoring for kidney health indicators
Blood pressure monitoring serves a dual purpose – high blood pressure damages kidneys while kidney disease raises blood pressure. This creates a dangerous cycle where each condition worsens the other.
Regular blood pressure checks help catch hypertension before it causes irreversible kidney damage. Target blood pressure for kidney protection is typically below 130/80 mmHg, though your doctor may set different goals based on your individual risk factors.
Ambulatory blood pressure monitoring provides a complete picture by tracking readings over 24 hours. This catches “white coat hypertension” and nighttime blood pressure spikes that office visits miss.
Who Needs More Frequent Kidney Monitoring

Diabetics Requiring Specialized Screening Schedules
Diabetes significantly increases your risk of developing kidney disease, with diabetic nephropathy affecting about 40% of people with diabetes. If you have Type 1 diabetes, annual kidney screening should begin five years after your diagnosis. For Type 2 diabetes, screening should start immediately upon diagnosis since the disease may have been present for years before detection.
Your doctor will likely recommend testing every three to six months if you already show signs of kidney involvement. This includes monitoring your HbA1c levels alongside kidney function tests, as blood sugar control directly impacts kidney health. The screening becomes even more critical if your diabetes has been poorly controlled or if you’ve had the condition for more than 10 years.
Individuals with Family History of Kidney Disease
Genetics play a significant role in kidney disease development. If your parents, siblings, or grandparents had chronic kidney disease, polycystic kidney disease, or other hereditary kidney conditions, you’re at higher risk and need more vigilant monitoring.
Start discussing kidney health with your doctor in your twenties, even if you feel perfectly healthy. Many genetic kidney diseases develop slowly and silently. Polycystic kidney disease, for example, can remain undetected for decades while gradually damaging kidney tissue.
Your screening schedule should include annual blood tests and periodic imaging studies, especially if multiple family members were affected. Early detection can help you make lifestyle changes and receive treatments that slow disease progression significantly.
People with High Blood Pressure or Heart Disease
High blood pressure is both a cause and consequence of kidney disease, creating a dangerous cycle that can rapidly worsen both conditions. Your kidneys and cardiovascular system are intimately connected – what affects one directly impacts the other.
If you have hypertension, you need kidney function tests at least annually, and more frequently if your blood pressure isn’t well-controlled. The same applies if you have heart disease, heart failure, or have had a heart attack. These conditions often share common underlying causes and risk factors with kidney disease.
Your monitoring should include regular blood pressure checks, urine tests for protein, and blood tests for kidney function. Even mild elevations in these markers warrant closer observation, as cardiovascular and kidney diseases often progress together.
Those Taking Medications That Affect Kidney Function
Many common medications can damage your kidneys over time, especially when used regularly or in high doses. NSAIDs like ibuprofen and naproxen top this list, particularly dangerous when used daily for chronic pain or arthritis.
If you take blood pressure medications called ACE inhibitors or ARBs, regular monitoring is essential to ensure they’re helping rather than harming your kidneys. While these medications often protect kidney function, they can occasionally cause problems in certain individuals.
Antibiotics, chemotherapy drugs, and some supplements also require careful kidney monitoring. Keep a complete list of all medications and supplements you take, and discuss kidney-safe alternatives with your doctor when possible. Your screening frequency may need to increase to every three to six months depending on your medication regimen and kidney function baseline.
Your kidneys work tirelessly behind the scenes, filtering waste and keeping your body balanced, but kidney disease often develops silently without obvious symptoms. Catching problems early through regular checkups can mean the difference between managing a condition effectively and facing serious health complications down the road. Simple blood and urine tests can reveal kidney damage long before you feel unwell, giving you and your doctor the chance to take action when treatments work best.
Don’t wait until symptoms force your hand – talk to your doctor about including kidney function tests in your routine health screenings, especially if you have diabetes, high blood pressure, or a family history of kidney problems. Your kidneys deserve the same attention you give your heart and other vital organs. Schedule that checkup today and take control of your kidney health before problems have a chance to take control of your life.

Comments are closed